
How Self-Insured Entities Can Take Action to Address Spiraling Expenses
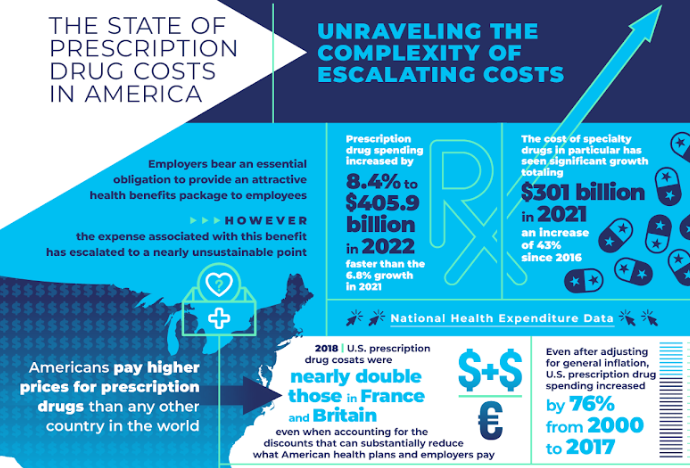
Employers bear an essential obligation to provide an attractive health benefits package to employees. However, the expense associated with this benefit has escalated to a nearly unsustainable point. The Center for American Progress identifies a significant factor contributing to this increasing cost as the exploitation of the prescription drug patent system. They highlight how drug manufacturers, PBMs, and large systems leverage their market power to force insurance carriers into “increasingly aggressive contract terms and prices.” Ultimately, it’s the health plan purchasers, the employers, who absorb these price hikes, with a portion of the expenses subsequently passed along to employees.
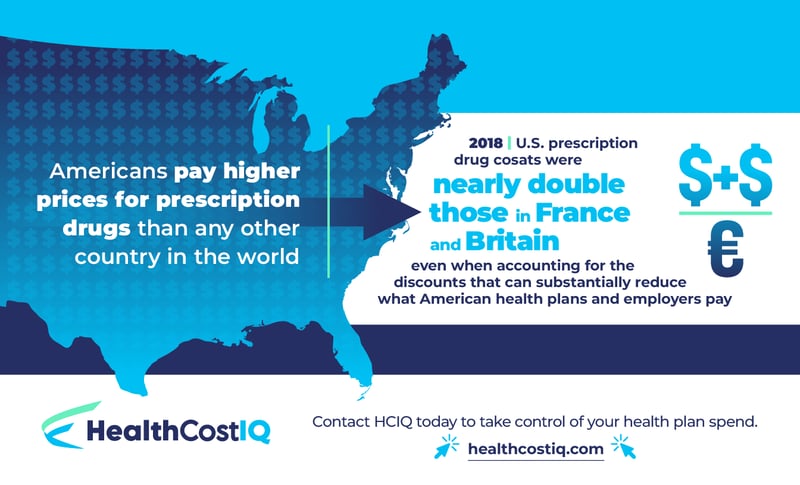
According to National Health Expenditure Data, prescription drug spending increased by 8.4% to $405.9 billion in 2022, faster than the 6.8% growth in 2021. The cost of specialty drugs, in particular, has seen significant growth, totaling $301 billion in 2021, an increase of 43% since 2016. While these drug costs are a notable hit to a self-insured employer’s bottom line, it’s an ever-present burden for Americans as a whole, who pay higher prices for prescription drugs than any other country in the world.
Health Cost IQ and our comprehensive Pharmacy Opportunity Discovery Module help self-insured entities address this problem. In this post, we’ll dig deeper into the reason for the rising drug prices, what claims data can tell us, and how to use the insights provided by this data to cut costs. This investigative work can lead to significant savings not only for employers but for employees as well.
The Uphill Battle of Prescription Drug Costs
The New York Times ran an article in January 2024 outlining six reasons drugs in the United States cost so much. The article quotes Ameet Sarpatwari, an expert in pharmaceutical policy at Harvard Medical School, who shares that “The U.S. market is the bank for pharmaceutical companies.” In other words, our prescription drug system is known internationally to be broken and easy to exploit.
One of the issues noted by the Times is that our system for setting prices is fragmented and complicated. The article claims that “the system is so confusing that doctors and patients trying to decide between seemingly comparable drugs have no easy way to determine what their actual cost will be at the pharmacy counter.” Whereas other industrialized countries depend on a central negotiating body (usually their government) to determine drug prices, in the U.S., this decision is split between numerous health plans, leaving buyers little to no bargaining power.
Drug companies often defend high drug prices based on the expense of running clinical trials. And yet, studies show there’s little to no association between the costs for research and development and the market rate charged for these medications.
In light of the challenges, it may seem as though self-insured employers, professional employer organizations (PEOs), and educational consortiums have little hope of combating rising pharmaceutical costs. But there is good news—there is a way to fight back and reign in expenses.
Leveraging Pharmacy Drug Claims Data for Savings
While the reality is that pharmacy drug costs are steadily on the rise, it’s also true that addressable inefficiencies often occur within formularies. All too often, costly brand-name drugs are prescribed when lower-cost generic equivalents or lower-cost generic therapeutic alternatives are readily accessible. Armed with the right intelligence, self-insured entities and the companies that support them can customize their formularies in ways that target the use of the most cost-efficient drugs available.
HCIQ’s Pharmacy Opportunity Discovery module receives weekly updates detailing the cost of every single FDA-approved drug in the United States. Whatever the drug, we have access to the best price for that drug at any point in time. Our algorithms feed off this intelligence every time it’s refreshed and conduct comparisons against what our clients currently pay. As a result, our clients can continually monitor the best-case scenario price for the drugs they’re interested in, ensuring they have access to optimal pricing options at all times.
Comparing rates by month or year, it’s possible to identify inefficiencies in spending. Our clients can consider all the generic categories available that offer an alternative for the same chronic conditions with the same clinical efficacy of the name-brand drugs but at considerable savings. This intelligence, which is displayed in precise dollar amounts of savings opportunities, empowers clients to negotiate for formulary design changes that bring down their prescription drug costs.
The Takeaway
If your organization is grappling with the increasing burden of prescription drug expenses and is ready to address this issue with practical data and relevant insights, HCIQ is equipped to help. We’re committed to ensuring that you avoid unnecessary expenditures and effectively mitigate waste within your health plan. To learn more about how HCIQ can help you start saving money right away, set up a time to connect with a member of our team today. Contact HCIQ.
Fill out the form below to download our infographic, The State of Prescription Drug Costs in America.


Leave Your Comment Here